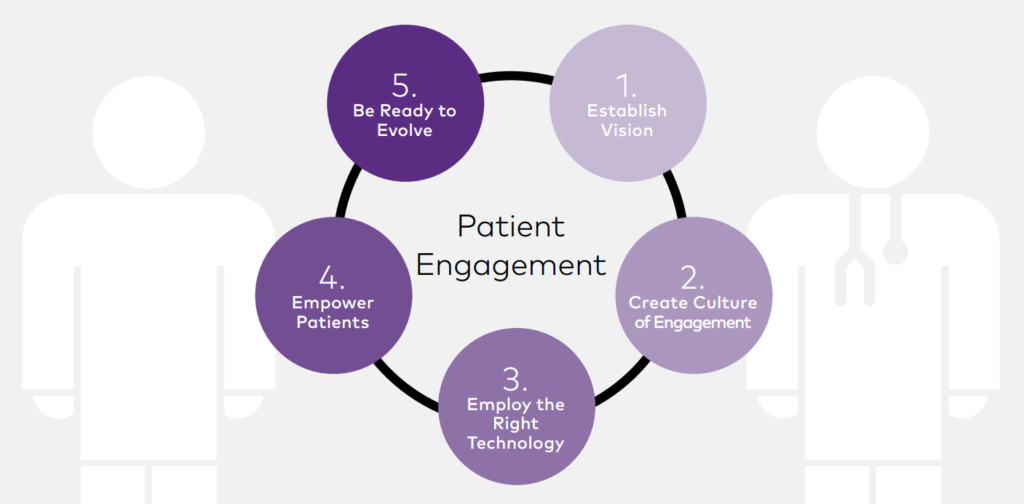
What is Patient Engagement in Healthcare?
Patient engagement in Healthcare is more than just a buzzword in today’s healthcare landscape—it’s a pivotal component of delivering high-quality, personalized care. At its core, patient engagement refers to the active participation of patients in their own health and wellness journey. It involves a two-way partnership where patients are not just passive recipients of care but are well-informed, involved, and motivated participants. Whether it’s making decisions about treatment options, managing chronic conditions, or adopting healthier lifestyles, engaged patients are more likely to follow through and take control of their health outcomes.
Think of patient engagement as a relationship—one built on trust, communication, and collaboration. Healthcare professionals provide the guidance and tools, but patients must be equally invested in their care. This relationship creates a shared sense of responsibility, where both parties work together towards better health outcomes.
In today’s data-driven era, patient engagement is facilitated by tools like patient portals, mobile apps, wearable devices, and telehealth platforms. These technologies offer real-time access to health records, medication reminders, appointment scheduling, and even direct communication with providers. But it’s not just about tech—it’s about fostering an environment where patients feel empowered to ask questions, seek information, and make decisions that align with their values and preferences.
Why It Matters in Modern Healthcare
Patient engagement in healthcare isn’t just a feel-good strategy; it’s a proven driver of better health outcomes and lower costs. Engaged patients are more likely to adhere to treatment plans, attend follow-up appointments, and manage chronic diseases more effectively. That translates into fewer hospitalizations, reduced emergency room visits, and a lower risk of complications.
Moreover, in value-based care models, where reimbursement is tied to outcomes rather than procedures, engaging patients becomes a critical success factor. Providers who build strong relationships with their patients can expect higher satisfaction scores, better clinical results, and increased patient loyalty.
From a societal perspective, engaged patients also lead to more sustainable healthcare systems. When individuals understand their health risks and take preventive actions, it eases the burden on hospitals and clinics. Engagement shifts the focus from sick care to health care—a proactive, preventive approach that benefits everyone.
In short, mastering patient engagement isn’t optional; it’s essential for delivering care that’s not just clinically effective but also compassionate, personalized, and forward-thinking.
The Evolution of Patient Engagement
Traditional vs. Modern Approaches
Back in the day, healthcare followed a paternalistic model—doctors made decisions, and patients followed orders. There wasn’t much room for dialogue or shared decision-making. Fast forward to today, and the dynamic has flipped. Patients are demanding more transparency, access, and involvement in their care. Thanks to the internet and digital health tools, they’re more informed than ever before. And with that knowledge comes the expectation of being treated as partners rather than passive participants.

In the traditional model, appointments were brief, information was limited, and decisions were top-down. Modern approaches emphasize longer consultations, collaborative care planning, and personalized support. Now, doctors are educators and advisors, helping patients understand their options and empowering them to take the lead in their healthcare journey.
The shift didn’t happen overnight. It was fueled by a mix of policy changes, technological advancements, and growing awareness about patient rights. The Affordable Care Act (ACA), for example, emphasized patient-centered care as a key element of healthcare reform. Alongside that, digital tools like electronic health records (EHRs) and patient portals gave people more control over their medical information.
As healthcare continues to evolve, patient engagement will remain at the heart of this transformation—bridging the gap between care providers and the people they serve.
Impact of Technology on Patient Interaction
Technology has completely revolutionized how patients interact with the healthcare system. Just a few decades ago, booking an appointment meant making a phone call during business hours, and accessing your medical records required formal requests and paperwork. Today, it’s as simple as tapping an app.
Digital tools have democratized healthcare information. Patients can now view lab results in real-time, message their doctors directly, and even attend virtual appointments from the comfort of their homes. This kind of convenience not only improves satisfaction but also makes it easier for people to stay engaged with their care.
Wearable devices like smartwatches and fitness trackers allow patients to monitor their health continuously—tracking steps, sleep patterns, heart rate, and more. For providers, this data offers valuable insights into a patient’s lifestyle and helps tailor care plans accordingly.
But it’s not all smooth sailing. While tech has its perks, it also introduces new challenges like data privacy concerns, information overload, and disparities in access. That said, when used effectively, technology is one of the most powerful tools in the patient engagement toolkit. It breaks down barriers, improves communication, and supports a more proactive, connected approach to healthcare.
Core Principles of Patient Engagement
Shared Decision-Making
Shared decision-making (SDM) is the gold standard of modern patient care. It’s a collaborative process where clinicians and patients work together to make healthcare decisions that align with the patient’s values, preferences, and lifestyle. Instead of being told what to do, patients are presented with options, risks, benefits, and supported in making choices that feel right for them.
This principle acknowledges that while healthcare professionals bring medical expertise to the table, patients bring their lived experiences. They know their bodies, their challenges, and their goals. Merging these perspectives results in more tailored, effective care.
SDM is especially important in cases where there’s no one “right” answer—like managing chronic conditions or choosing between different treatment routes. It fosters trust, improves satisfaction, and leads to better adherence to care plans because patients feel a sense of ownership over their decisions.
Implementing SDM requires time, communication skills, and often decision aids like charts, videos, or apps to help explain complex information. But the payoff is worth it—engaged patients who are informed and confident in their healthcare choices.
Empowerment Through Education
Education is the cornerstone of patient empowerment. When people understand their health conditions, treatment options, and preventive strategies, they’re better equipped to take control of their well-being. Unfortunately, health literacy remains a significant barrier for many. Studies show that a large percentage of adults struggle to comprehend even basic medical instructions, let alone complex treatment plans.
To bridge this gap, healthcare providers must commit to simplifying and personalizing educational efforts. That means ditching the jargon and delivering clear, actionable information through various formats—verbal instructions, printed materials, videos, infographics, and even interactive tools. Every patient learns differently, so offering diverse educational mediums ensures greater reach and comprehension.
Moreover, education shouldn’t stop after a diagnosis or discharge. Ongoing learning opportunities like workshops, webinars, support groups, and online resources play a crucial role in sustaining engagement. When patients continue to learn, they stay connected and committed to their care goals.
Education also helps build trust. When providers take the time to explain conditions, medications, and procedures thoroughly, patients feel valued and respected. That trust, in turn, makes them more likely to speak up, ask questions, and follow medical advice. Bottom line: educated patients are engaged patients.
Personalization of Care
No two patients are the same, so why should their care plans be? Personalization is a key pillar of effective patient engagement. It’s about recognizing the unique needs, preferences, lifestyles, and cultural backgrounds of each individual—and tailoring care accordingly.
This goes beyond customizing treatment plans. It includes considering how patients prefer to receive information (email vs. phone vs. in-person), what language they speak, what social or financial barriers they might face, and even what motivates them to stay healthy. For example, a tech-savvy millennial might respond well to a fitness app, while a senior patient might prefer printed health tips and regular phone check-ins.
Personalization builds stronger patient-provider relationships. When people feel seen and understood, they’re more likely to engage in meaningful dialogue and trust the care they’re receiving. It also increases compliance. Patients are much more likely to stick to a treatment regimen that fits into their daily lives rather than disrupts them.
Technology makes personalization easier than ever. Electronic health records (EHRs), predictive analytics, and patient surveys can all be used to gather data and insights that shape individualized care experiences. However, human connection still plays a vital role. Listening to patients, showing empathy, and adjusting approaches based on feedback ensures that personalization is authentic and effective.
Benefits of Effective Patient Engagement
Improved Health Outcomes
There’s plenty of evidence that shows engaged patients experience better health outcomes. Why? Because involvement drives accountability and action. When patients understand their conditions and actively participate in their care, they’re more likely to adhere to medication schedules, follow lifestyle recommendations, and attend follow-up visits. All these behaviors lead to more consistent management of chronic diseases, quicker recovery times, and lower chances of hospital readmission.
Engaged patients also tend to recognize symptoms earlier and seek timely help, which can be crucial in preventing complications. In preventive care, education and engagement lead to increased screening rates, vaccinations, and healthier daily habits.
These outcomes aren’t just numbers on a chart—they represent real improvements in quality of life. Patients feel better physically, mentally, and emotionally when they’re in control of their health journey.
Increased Patient Satisfaction
Patients who feel involved in their healthcare decisions are generally happier with the care they receive. That satisfaction comes from being heard, respected, and included. It also stems from improved communication, quicker responses to concerns, and clearer expectations.
Engagement creates a feedback loop of positivity. Satisfied patients are more likely to return for future care, recommend the provider to others, and give favorable reviews. For healthcare organizations, that means better reputation, higher patient retention, and even improved performance metrics tied to reimbursement models.
In fact, many healthcare systems now measure patient satisfaction as a key quality indicator. Investing in engagement isn’t just the right thing to do—it’s also a smart business strategy.

Reduced Healthcare Costs
When patients take preventive actions and manage chronic conditions effectively, it reduces the need for costly interventions like emergency room visits, hospital admissions, and long-term treatments. That has a direct impact on healthcare spending, both for individuals and the system as a whole.
For providers operating under value-based care models, this is a game-changer. They can reduce expenses while improving quality, leading to greater efficiency and financial incentives from payers.
From the patient’s perspective, engagement can mean fewer co-pays, less time off work, and a better understanding of insurance and treatment options—all of which contribute to financial peace of mind.
Strategies to Improve Patient Engagement
Communication is Key
You can’t engage patients if you’re not communicating effectively. It’s the foundation of every relationship in healthcare. Clear, empathetic, and consistent communication helps build trust, reduce anxiety, and encourage patients to be active participants in their care.
That starts with listening. Providers need to create space for patients to express concerns, ask questions, and share personal experiences. It’s about moving from a lecture-style visit to a true conversation.
Language is also critical. Avoiding complex medical terms and using plain language makes instructions easier to understand and follow. Visual aids, metaphors, and analogies can also help explain complicated concepts in relatable ways.
Beyond face-to-face interactions, communication should continue across various platforms—phone calls, emails, texts, patient portals, and even social media. Multichannel communication ensures that patients stay informed and connected throughout their care journey.
Read Alos : Plastic Surgery SEO Strategies for 2025: Dominate Local Search Results
Leveraging Digital Tools and Portals
Patient portals and mobile health apps are powerful tools for boosting patient engagement. These platforms give patients direct access to their medical records, test results, medication lists, and appointment scheduling. They also allow secure messaging with healthcare teams, enabling quick clarification of doubts and better coordination.
Digital tools offer a level of convenience and transparency that fosters trust and involvement. When patients can check their own data and interact with their care teams at any time, they’re more likely to feel in control.
Beyond portals, there are apps for medication reminders, symptom tracking, nutrition planning, and even mental health support. These tools can be tailored to individual needs and preferences, creating a highly personalized care experience.
However, it’s important to ensure these tools are user-friendly and accessible to all patients, regardless of age or tech proficiency. Training and support should be available to help patients make the most of these resources.
Role of Healthcare Providers in Patient Engagement
Providers play a critical role in setting the tone for patient engagement. It starts with attitude—approaching care as a partnership rather than a transaction. Providers must foster an environment where patients feel safe, respected, and encouraged to take an active role.
That means being approachable, empathetic, and attentive during every interaction. It also involves guiding patients through their care journey, helping them set realistic goals, and celebrating their progress along the way.
Engagement also requires time—a scarce resource in busy clinics. But even short interactions can be meaningful when they’re focused and intentional. Providers can use tools like decision aids, handouts, and follow-up calls to extend the engagement beyond the exam room.
Ultimately, it’s about creating a culture of care that values collaboration. When healthcare professionals commit to this mindset, patient engagement becomes a natural, rewarding part of the care process.
Role of Technology in Patient Engagement
Mobile Apps and Wearables
Mobile health (mHealth) apps and wearable devices have drastically transformed how patients monitor and manage their health. These technologies allow for real-time tracking of vital signs, physical activity, nutrition, and medication adherence—all from the convenience of a smartphone or smartwatch.
For instance, someone managing diabetes can use a mobile app to log blood glucose levels, track their meals, and receive alerts for insulin. A cardiac patient might wear a smartwatch that monitors heart rate and detects arrhythmias, alerting both the patient and their care provider instantly. These tools foster continuous patient engagement, far beyond the walls of a doctor’s office.
What makes these technologies particularly powerful is their ability to provide instant feedback. Patients receive reminders, encouragement, and even gamified achievements that make managing health feel more interactive and rewarding.
However, accessibility and data privacy are key concerns. Not every patient can afford or comfortably use these technologies. And with more health data floating around in the cloud, providers and app developers must prioritize security and clear consent protocols. Still, when implemented thoughtfully, wearables and apps are among the most impactful innovations driving patient engagement today.
Telemedicine and Remote Monitoring
Telemedicine has exploded in popularity—especially since the COVID-19 pandemic—and it’s here to stay. With virtual visits, patients can consult with their healthcare providers from virtually anywhere. This convenience is particularly beneficial for those in rural areas, people with mobility issues, and busy professionals who struggle to attend in-person appointments.
But it’s not just about convenience. Telemedicine fosters more consistent and timely communication, which is vital for managing chronic conditions, mental health, and preventive care. It also opens the door for interdisciplinary collaboration, allowing multiple specialists to be involved in a patient’s care plan without the logistical nightmare of scheduling in-person consultations.
Remote monitoring tools take it a step further by enabling providers to track patients’ health data continuously. For example, blood pressure cuffs, glucose monitors, and oxygen sensors can transmit real-time data to care teams. If any red flags appear, interventions can happen faster, preventing serious complications and improving outcomes.

These technologies empower patients to take responsibility for their health while providing clinicians with better insights to guide decision-making. It’s a win-win for engagement and care efficiency.
AI and Chatbots in Patient Support
Artificial Intelligence (AI) and chatbots are becoming the silent partners in healthcare patient engagement. These tools help answer patient queries, schedule appointments, send medication reminders, and provide personalized health tips—all 24/7.
Imagine a patient waking up at 2 a.m. with a question about their medication. Instead of waiting until morning to call a nurse, they can type into a chatbot that instantly pulls up the answer from a trusted database. That’s not just convenient—it’s empowering.
AI also powers predictive analytics that help identify at-risk patients and intervene before issues escalate. It can analyze EHRs, past visits, lifestyle data, and more to flag trends and guide early action.
However, AI is still evolving. It should complement—not replace—the human touch in healthcare. Emotional intelligence, empathy, and nuanced judgment remain the domain of human providers. But as a support system, AI significantly enhances patient engagement by making healthcare more responsive and accessible.
Measuring Patient Engagement
Key Performance Indicators (KPIs)
You can’t improve what you don’t measure. That’s why tracking KPIs is essential for evaluating patient engagement initiatives. Some common metrics include:
- Portal logins and usage frequency
- Appointment adherence and follow-up rates
- Medication refill and adherence tracking
- Participation in wellness programs
- Patient-reported outcomes and satisfaction surveys
These indicators give providers a snapshot of how involved patients are in their care. They also help identify which strategies are working and where gaps exist.
KPI tracking should be ongoing and dynamic. As engagement tools and patient needs evolve, so should the metrics used to evaluate them. Data transparency is also important—sharing engagement results with staff and patients fosters accountability and a shared commitment to improvement.
Patient Feedback and Surveys
There’s no better source of insight than the patients themselves. Regular feedback through surveys, interviews, focus groups, and reviews offers a goldmine of information on how to improve engagement.
Ask the right questions: Do patients feel heard during appointments? Are educational materials helpful? Is the technology easy to use? The more specific the feedback, the more actionable it becomes.
But don’t just collect feedback—act on it. When patients see that their opinions lead to real changes, it strengthens trust and boosts future engagement.
Surveys should be short, accessible, and offered in multiple languages and formats (digital, paper, phone) to reach all demographics. And always follow up—let patients know what changes were made based on their input.
Data Analytics in Patient Behavior
Advanced analytics can transform raw data into meaningful insights. By analyzing trends in patient behavior—like missed appointments, portal logins, or response to treatment plans—healthcare organizations can tailor their engagement strategies to meet specific needs.
Predictive models can help identify which patients are most at risk of disengaging or facing health deterioration. This proactive approach allows care teams to intervene early with support, education, or outreach.
Analytics can also reveal disparities in engagement among different populations. Maybe older patients are less likely to use digital tools, or non-English speakers struggle with educational content. Identifying these gaps enables targeted interventions that promote equity and inclusion.
In essence, data analytics helps take the guesswork out of engagement. It offers a roadmap for more personalized, efficient, and impactful patient interaction.
Challenges in Patient Engagement
Cultural and Language Barriers
Cultural norms, beliefs, and language differences can significantly impact how patients interact with the healthcare system. For instance, in some cultures, it may be taboo to question a doctor’s opinion, while in others, family consensus is more important than individual decision-making.
Language can also be a major barrier. If patients can’t fully understand what their provider is saying—or if there’s no translated material—they’re less likely to engage. Miscommunication leads to confusion, mistrust, and poor adherence.
To overcome this, healthcare organizations must invest in culturally competent care. That means hiring diverse staff, providing interpreter services, and tailoring education materials to different languages and literacy levels. Training providers in cultural sensitivity and inclusive communication techniques is also crucial.
Understanding and respecting a patient’s background creates a safe space for open dialogue and collaboration. When patients feel seen and heard, engagement naturally follows.
Read Also : SEO for Doctors: Proven Tactics to Rank #1 and Grow Your Practice in 2025
Digital Divide and Accessibility
While digital tools offer great promise, not everyone has equal access to them. Many rural, low-income, and elderly patients lack smartphones, reliable internet, or tech literacy. This digital divide can widen disparities in care and engagement.
Healthcare systems must ensure that engagement strategies are inclusive. That might mean offering low-tech options like phone calls, printed materials, or in-person support. It also involves providing digital literacy training and investing in community resources like public internet kiosks or lending programs for devices.
Accessibility goes beyond tech—it includes physical, cognitive, and language accessibility. Every patient, regardless of ability or background, should be able to participate fully in their care.
Trust and Data Privacy Issues
Engagement relies heavily on trust. If patients are concerned about how their data is used—or feel that their privacy isn’t protected—they’re less likely to engage with digital tools or share important information.
Building trust starts with transparency. Healthcare organizations must clearly explain how patient data is collected, stored, and protected. They should also offer easy-to-understand consent forms and give patients control over their data sharing preferences.
Beyond privacy, trust also hinges on consistent, respectful care. Patients are more likely to engage when they believe their provider has their best interests at heart. It’s a long-term relationship that must be nurtured with honesty, integrity, and communication.
Building a Patient-Centric Culture
Training Healthcare Staff
Creating a culture centered on patient engagement starts with the people who provide care. Healthcare staff—doctors, nurses, administrative workers, and even janitors—play a role in shaping the patient experience. That’s why consistent training in communication, empathy, and cultural competence is non-negotiable.
It’s not just about teaching new skills; it’s about shifting mindsets. Staff must understand that patients are not just charts or appointment slots—they’re individuals with fears, goals, and questions. Training programs should focus on active listening, emotional intelligence, and strategies to involve patients in their care decisions.
Ongoing professional development helps keep staff aligned with best practices. Role-playing, peer mentoring, and feedback loops can strengthen these skills over time. When everyone is on the same page, patients feel the difference—more warmth, more clarity, more trust.
When patients walk into a facility and every interaction feels human, helpful, and respectful, patient engagement becomes a natural part of the experience, not a forced initiative.
Creating Inclusive Environments
Inclusivity is a key pillar of a patient-centric culture. Healthcare environments must feel welcoming and safe for all, regardless of race, gender, age, ability, or background. That includes everything from how signage is written to how intake forms are designed.
Small details make a big impact. Are there gender-inclusive options on forms? Is there wheelchair access and assistance for those with limited mobility? Are materials available in multiple languages and at different reading levels? These details speak volumes about how much an organization values its patients.
An inclusive environment also means being aware of unconscious bias. Staff should be trained to recognize and challenge assumptions that can interfere with care—whether it’s judging someone based on appearance or dismissing symptoms due to stereotypes.
Inclusivity builds trust, and trust leads to engagement. When patients feel accepted and understood, they’re far more likely to participate fully in their care.
Policies Supporting Engagement
Patient engagement must be supported by policy—not just promoted through posters and slogans. Healthcare organizations should embed engagement into their operational standards, from hiring practices to care protocols to performance evaluations.
That might mean creating policies that require shared decision-making practices, mandating patient satisfaction surveys, or tying bonuses to engagement metrics. It also includes policies on digital access, like ensuring that telehealth services meet privacy standards and accessibility needs.
Leadership must be fully committed. When executives prioritize engagement, allocate resources to support it, and model collaborative behavior, it sets the tone for the entire organization.
Policies should be regularly reviewed and updated based on patient feedback and evolving best practices. This keeps the engagement strategy responsive, agile, and effective.
Future Trends in Patient Engagement
Predictive Analytics and Personalization
The future of patient engagement is all about anticipation. Predictive analytics uses historical data, behavior patterns, and clinical insights to foresee what a patient might need before they even ask.
For instance, if data shows that a patient with diabetes often misses medication refills around payday, a system can proactively send reminders or offer financial aid options. These small interventions, powered by big data, can prevent bigger health issues down the line.
Personalization will also reach new heights. Engagement tools will be able to recommend diet changes, suggest appointment times, or adjust communication styles based on each patient’s unique habits and preferences.
This proactive, data-driven approach will make healthcare more responsive and relevant, keeping patients more engaged and empowered.
Integration of AI in Healthcare
AI is poised to be the backbone of future engagement strategies. Beyond chatbots and reminders, AI will soon assist with real-time diagnostics, monitor emotional well-being, and recommend customized treatment plans.
Imagine a virtual health assistant that knows your medical history, anticipates your symptoms, and coaches you through daily health decisions. That’s not sci-fi—it’s where we’re heading.
But for AI to truly enhance engagement, it must be ethical, transparent, and inclusive. Algorithms should be free of bias, and patients should understand how AI tools impact their care. When used responsibly, AI can streamline care and keep patients connected in powerful ways.
Holistic and Preventative Care Models
The future of engagement also lies in shifting from reactive to proactive care. Instead of just treating illness, healthcare will focus more on preventing it—and that requires deep, ongoing engagement.
Holistic care models consider the whole person—not just physical symptoms but also mental health, lifestyle, environment, and social factors. Patients will be guided not just to heal, but to thrive.
Expect to see more wellness coaching, behavioral health integration, community outreach programs, and lifestyle medicine. These models promote long-term engagement because they make patients feel supported in all aspects of life—not just when they’re sick.
Case Studies of Successful Patient Engagement
Magical clinic’s Digital Engagement Journey
Magical CLINIC , a mid-sized Medical Tourism Company in turkey, transformed patient engagement by launching a comprehensive digital health platform. The portal allowed patients to view medical tourism packages , speak with doctors, send test results, book appointments, and communicate with providers 24/7.
The results? A 30% reduction in no-show appointments, a 45% increase in patient satisfaction scores, and improved medication adherence rates. Patients reported feeling more in control and more connected to their care teams.
Magical Clinic also offered tutorials and phone support to help less tech-savvy patients get comfortable with the system. Their inclusive approach made digital tools work for everyone—not just the young or tech-literate.
Clinic B’s Patient-Centered Programs
Clinic Emilly, a rural family practice, focused on face-to-face engagement. They introduced “care coaches”—nurses trained to follow up with patients post-visit to check on progress, explain medications, and offer emotional support.
They also ran community health classes on managing diabetes, heart disease, and mental health. These free workshops turned passive patients into active learners and created a sense of community support.
In just 18 months, Clinic Emilly saw a drop in ER visits and a rise in patient retention. It proved that even without fancy tech, personal connection drives powerful engagement.
How to Get Started with Patient Engagement
Assess Current Practices
Before diving into new strategies, it’s crucial to evaluate what’s currently working—and what’s not. Are patients missing appointments? Are survey scores low? Is your portal underused?
Gather data, hold internal audits, and get feedback from both staff and patients. This baseline helps you identify gaps and opportunities for improvement.
Set Clear Goals and Objectives
You can’t measure success without a target. Define what you want to achieve—whether it’s improved adherence, better satisfaction scores, or increased portal use. Make goals specific, measurable, and time-bound.
Involve your team in setting these goals. When staff feels ownership, they’re more invested in achieving them.
Implement and Monitor Progress
Start with a few high-impact changes—like staff training, a better intake process, or launching a text reminder system. Keep it manageable, then scale up as you learn what works.
Track progress regularly, adjust based on results, and celebrate small wins along the way. Engagement is a journey, not a one-time fix.
Patient Engagement for Special Populations
Pediatric Patient Engagement
Kids require a different approach to engagement. Education must be fun and age-appropriate, and communication often involves parents or guardians. Animated videos, interactive games, and rewards can turn doctor visits into positive learning experiences.
Providers should focus on building trust early—using simple words, explaining procedures, and creating a friendly environment. The goal is to make kids feel safe and involved, not scared or confused.
Geriatric and Chronic Care Management
Older adults often deal with multiple health issues, medications, and care providers. Engagement here means simplifying care, ensuring clarity, and offering support systems.
This might involve print materials in large fonts, scheduled check-in calls, and involving caregivers in appointments. Geriatric engagement must also address mental health and mobility challenges.
For patients with chronic illnesses, regular contact and tailored education help keep them on track. Group support, lifestyle coaching, and remote monitoring are all effective tools.
The Role of Family and Caregivers
Partnering with Caregivers
Family members and caregivers often play a crucial role in a patient’s care. Engaging them means sharing information, respecting their insights, and offering tools to support their loved ones.
Caregivers should be seen as allies, not outsiders. They help manage medications, attend appointments, and notice early signs of trouble.
Communication and Support Systems
Healthcare systems should provide caregivers with access to educational resources, appointment scheduling, and care updates. This improves coordination and reduces stress for everyone involved.
Support groups, respite care, and mental health resources for caregivers are also essential. When caregivers are supported, they’re better able to support the patient.
Conclusion
Patient engagement isn’t just a checkbox in healthcare—it’s the foundation of better outcomes, stronger relationships, and a more compassionate care system. By focusing on communication, education, personalization, and technology, providers can turn passive patients into empowered partners.
The journey to mastering patient engagement takes time, commitment, and a willingness to adapt. But the payoff is well worth it: healthier people, happier communities, and a healthcare system that truly works for everyone.